Linking gut health to rheumatoid arthritis has been a topic of growing interest in the medical community. Research has shown a strong connection between the health of the gut microbiome and the development and progression of rheumatoid arthritis. The gut is home to trillions of bacteria that play a crucial role in regulating the immune system, inflammation, and overall health. An imbalance in the gut flora, known as dysbiosis, has been linked to various autoimmune diseases, including rheumatoid arthritis.
Key Takeaways:
- Gut microbiome: The balance of good and bad bacteria in the gut can play a significant role in the development and progression of rheumatoid arthritis.
- Leaky gut: Increased intestinal permeability, known as leaky gut, can trigger inflammation in the body, which can exacerbate rheumatoid arthritis symptoms.
- Immune system response: The gut is closely linked to the immune system, and imbalances in the gut can lead to an overactive immune response, contributing to the development of autoimmune diseases like rheumatoid arthritis.
- Diet and gut health: A healthy diet rich in fiber, probiotics, and prebiotics can promote a healthy gut microbiome and help reduce inflammation associated with rheumatoid arthritis.
- Probiotics and supplements: Certain probiotics and supplements may help restore a healthy balance of gut bacteria and reduce inflammation in individuals with rheumatoid arthritis.
- Consultation with a healthcare professional: It is important for individuals with rheumatoid arthritis to consult with a healthcare professional before making significant changes to their diet or adding supplements to their routine.
- Personalized treatment approach: Understanding the link between gut health and rheumatoid arthritis can help healthcare providers develop more personalized and effective treatment plans for patients.
Understanding Rheumatoid Arthritis
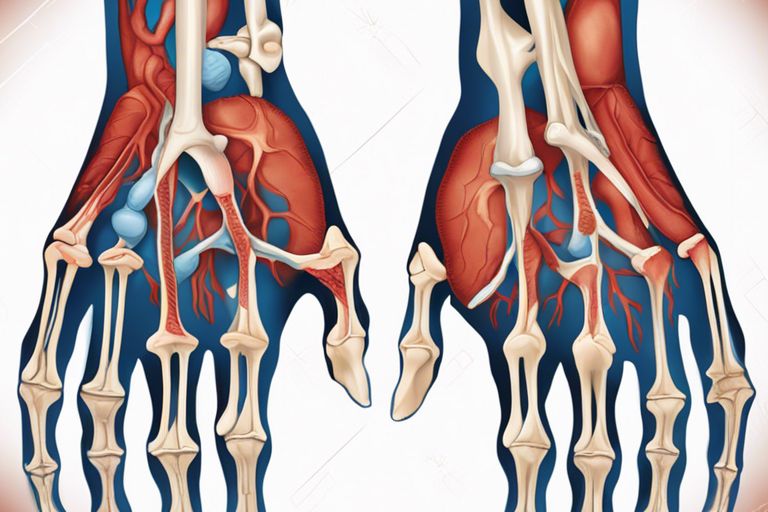
Even though arthritis is commonly associated with aging, rheumatoid arthritis is an autoimmune disease that can affect people of all ages. It is a chronic inflammatory disorder that primarily targets the joints, causing pain, swelling, and stiffness. The immune system mistakenly attacks the body’s own tissues, leading to inflammation in the lining of the joints and eventually causing damage to cartilage and bone.
Arthritis can lead to deformity and disability if left untreated. It affects not only the joints but can also impact other organs and systems in the body. Understanding the nature of rheumatoid arthritis is crucial for timely diagnosis and effective management of the condition.
Defining Rheumatoid Arthritis
With an estimated 1.3 million Americans living with rheumatoid arthritis, it is important to recognize the key characteristics of this condition. Rheumatoid arthritis is different from other forms of arthritis, such as osteoarthritis, as it is an autoimmune disease. The immune system attacks the synovium, the lining of the membranes that surround the joints, leading to inflammation and joint damage.
Rheumatoid arthritis is symmetrical, meaning it usually affects both sides of the body simultaneously. Common symptoms include joint pain, swelling, stiffness, and fatigue. If left untreated, rheumatoid arthritis can progress rapidly, causing irreversible damage to the joints.
Symptoms and Diagnosis
With rheumatoid arthritis, early diagnosis is crucial for preventing the progression of the disease and minimizing joint damage. Symptoms vary from person to person but commonly include joint pain and swelling, stiffness, and fatigue. These symptoms are typically worse in the morning or after periods of inactivity.
Current Treatment Options
Current treatment options for rheumatoid arthritis focus on reducing inflammation, alleviating symptoms, and preventing joint damage. Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), and biologic agents are commonly used to manage the disease. In some cases, surgery may be recommended to repair severely damaged joints.
Research into new treatment options, including targeted therapies and personalized medicine, is ongoing to improve outcomes for individuals with rheumatoid arthritis. Early intervention and a multidisciplinary approach involving healthcare providers such as rheumatologists, physical therapists, and occupational therapists are necessary for effective disease management.

The Gut Microbiome: A Complex Ecosystem
Unlike other parts of the body, the gut houses a vast and diverse community of microorganisms known as the gut microbiome. This complex ecosystem is made up of trillions of bacteria, fungi, viruses, and other microorganisms that play a crucial role in maintaining the overall health of the host.
Composition of the Gut Microbiome
One of the key aspects of the gut microbiome is its composition, which varies greatly from person to person. The types and proportions of microorganisms present in the gut can be influenced by a variety of factors such as diet, genetics, age, and environment. Despite this variability, several dominant bacterial phyla are commonly found in the gut, including Firmicutes, Bacteroidetes, Actinobacteria, and Proteobacteria.
Research has shown that a diverse and balanced gut microbiome is vital for maintaining optimal health. Disruptions in the composition of the gut microbiome, known as dysbiosis, have been linked to a range of health conditions, including autoimmune diseases like rheumatoid arthritis.
Factors Influencing Gut Microbiome Diversity
One of the factors that can influence the diversity of the gut microbiome is diet. A diet high in fiber and plant-based foods has been shown to promote the growth of beneficial bacteria in the gut, while a diet high in processed foods and sugar can lead to an imbalance in the microbiome.
Other factors that can impact gut microbiome diversity include antibiotic use, stress, environmental toxins, and lifestyle choices. It is important to note that these factors can have both positive and negative effects on the gut microbiome, underscoring the importance of maintaining a healthy lifestyle to support gut health.
The Immune System and Gut Microbiota Interplay
The Role of Gut Microbiota in Immune System Function
To understand the link between gut health and rheumatoid arthritis, we must explore into the intricate interplay between the immune system and the gut microbiota. An abundance of research has highlighted the crucial role of gut microbiota in regulating immune responses. The gut is home to trillions of microorganisms that play a pivotal role in maintaining immune homeostasis and fending off pathogens.
These commensal microbes interact with immune cells in the gut-associated lymphoid tissue, influencing the development and function of immune cells. Through various mechanisms, the gut microbiota helps educate the immune system, promoting tolerance to beneficial microbes while mounting appropriate responses against harmful invaders.
Dysbiosis and Immune Dysregulation
MicrobiotaDysbiosis refers to an imbalance in the gut microbiota composition, which can disrupt the delicate equilibrium between commensal and pathogenic microbes. This imbalance can lead to immune dysregulation, triggering inflammatory responses and contributing to the development of autoimmune conditions such as rheumatoid arthritis.
It is crucial to note that dysbiosis-induced immune dysregulation can manifest systemically, affecting not only the gut but also distant sites like the joints. Understanding the mechanisms underlying this interaction is crucial for developing targeted interventions that restore gut microbial balance and modulate immune responses to alleviate rheumatoid arthritis symptoms.
Scientific Evidence Linking Gut Health to Rheumatoid Arthritis
Epidemiological Insights
Your arthritis may have a deeper connection to your gut health than previously thought. Epidemiological studies have revealed a strong association between gut health and the development of rheumatoid arthritis. Research shows that individuals with certain gut microbiota compositions are more prone to developing autoimmune conditions like rheumatoid arthritis. Individuals with imbalanced gut flora are at a higher risk of developing rheumatoid arthritis, indicating a potential key role of the gut in the onset of this chronic inflammatory condition.
Moreover, studies have demonstrated a higher prevalence of gastrointestinal symptoms in rheumatoid arthritis patients, suggesting a bidirectional relationship between the gut and joint health. The link between gut dysbiosis and systemic inflammation underscores the importance of maintaining a healthy gut microbiome for overall well-being, particularly in individuals at risk for autoimmune diseases like rheumatoid arthritis.
Mechanistic Studies on Gut-Joint Axis
AxisUnderstanding the mechanisms behind the gut-joint axis is crucial in unraveling the link between gut health and rheumatoid arthritis. Mechanistic studies have shown that the gut microbiota play a pivotal role in modulating immune responses and inflammation, which are central processes in the pathogenesis of rheumatoid arthritis. Imbalance in gut microbiota composition can trigger an inflammatory cascade that may contribute to the development and progression of rheumatoid arthritis.
Furthermore, research has indicated that gut-derived microbial byproducts, such as lipopolysaccharides, can enter the bloodstream and stimulate immune cells, leading to systemic inflammation and joint damage. This direct communication between the gut and joints highlights the intricate interplay between gut health and rheumatoid arthritis pathophysiology, offering new avenues for potential therapeutic interventions targeting the gut microbiome.
Any disruption in the delicate balance of the gut-joint axis can have profound implications for the development and progression of rheumatoid arthritis. Understanding the complex interconnections between gut health, immune responses, and joint inflammation is imperative in paving the way for innovative approaches to managing this debilitating autoimmune condition.
Dietary Influences on Gut Health and Rheumatoid Arthritis
Pro-Inflammatory vs. Anti-Inflammatory Diets
Influences on gut health play a significant role in the development and progression of rheumatoid arthritis (RA). Not all diets are created equal when it comes to their impact on inflammation in the body. A pro-inflammatory diet, high in processed foods, refined sugars, and unhealthy fats, can disrupt the balance of gut bacteria and contribute to the systemic inflammation that worsens RA symptoms.
On the other hand, an anti-inflammatory diet rich in fruits, vegetables, whole grains, and healthy fats can help influence gut health in a positive way. These foods provide imperative nutrients and antioxidants that support a healthy gut microbiome and reduce inflammation throughout the body, potentially easing symptoms of RA.
Prebiotics, Probiotics, and Dietary Interventions
Diets rich in prebiotics and probiotics have shown promise in supporting gut health and mitigating the symptoms of RA. Prebiotics are non-digestible fibers that serve as fuel for beneficial gut bacteria, while probiotics are live bacteria that can directly influence the balance of gut microbiota. Diets high in prebiotic-rich foods such as garlic, onions, and bananas, along with probiotic-rich foods like yogurt and kefir, can enhance the diversity and resilience of the gut microbiome.
To further support gut health and reduce inflammation associated with RA, dietary interventions such as eliminating food allergens or sensitivities, following an elimination diet, or working with a nutritionist to create a personalized nutrition plan can be beneficial. These interventions can help identify trigger foods that exacerbate symptoms and promote the consumption of nutrient-dense, gut-friendly foods that may alleviate inflammation and improve overall well-being.
Potential Therapeutic Approaches Targeting the Gut
Many studies have shown a strong link between gut health and rheumatoid arthritis, paving the way for potential therapeutic approaches that target the gut to manage this chronic inflammatory condition. By focusing on modulating the microbiome and exploring innovative treatments like fecal microbiota transplantation, researchers are uncovering promising avenues for improving the symptoms and progression of rheumatoid arthritis.
Microbiome Modulation Strategies
The microbiome, which consists of trillions of microbes residing in the gut, plays a crucial role in immune regulation and inflammation. Microbiome modulation strategies aim to restore microbial balance and enhance the diversity of beneficial bacteria to promote immune tolerance and reduce chronic inflammation. Probiotics, prebiotics, dietary interventions, and personalized microbiome-targeted therapies are being investigated as potential approaches to modulate the gut microbiome and improve outcomes in rheumatoid arthritis.
The intricate interplay between the gut microbiome and the immune system highlights the therapeutic potential of targeting the microbiome in rheumatoid arthritis management. By harnessing the power of microbiome modulation strategies, researchers are striving to develop personalized interventions that can address the underlying mechanisms of autoimmunity and inflammation in individuals with rheumatoid arthritis.
Fecal Microbiota Transplantation and Its Prospects
Transplantation is a promising therapeutic approach that involves transferring fecal microbiota from a healthy donor to a patient with the goal of restoring a healthy gut microbiome balance. Studies have shown that fecal microbiota transplantation can lead to significant improvements in inflammatory conditions by modulating immune responses and reducing disease activity.
Potential applications of fecal microbiota transplantation in rheumatoid arthritis management are currently being explored, with early research indicating positive outcomes in terms of reducing joint inflammation and improving clinical symptoms. As this innovative therapy continues to be investigated, its prospects in reshaping the gut microbiome and immune responses offer new hope for individuals living with rheumatoid arthritis.
Future Directions in Research and Treatment
Once again, the link between gut health and rheumatoid arthritis has opened up exciting avenues for future research and treatment possibilities. As we examine deeper into understanding the intricate relationship between the gut microbiome and autoimmune diseases, including rheumatoid arthritis, new insights are emerging that could revolutionize how we approach the management of this chronic condition.
Challenges and Opportunities in Gut Microbiome Research
Microbiome research presents both challenges and opportunities in unraveling the connection between gut health and rheumatoid arthritis. One of the main challenges is the complexity of the gut microbiome, which consists of trillions of bacteria with diverse functions. Understanding how specific bacterial populations influence the development and progression of rheumatoid arthritis requires sophisticated techniques and large-scale studies. However, advancements in technology and bioinformatics offer unprecedented opportunities to analyze the microbiome in greater detail than ever before.
Microbiome research also faces the challenge of variability among individuals and the lack of standardized protocols. To address these issues, collaboration among researchers from different fields is imperative to establish a comprehensive understanding of the gut microbiome’s role in rheumatoid arthritis. By working together, the scientific community can overcome these challenges and pave the way for innovative treatments targeting the microbiome to improve outcomes for patients.
Personalized Medicine and Holistic Approaches
The emerging field of personalized medicine holds great promise for the future of rheumatoid arthritis treatment. By tailoring therapies to individual patients based on their unique gut microbiome profiles, clinicians can potentially achieve more effective outcomes with fewer side effects. Integrating holistic approaches that consider not only the microbiome but also lifestyle factors, diet, and stress management can lead to a more comprehensive and personalized treatment plan for patients with rheumatoid arthritis.
Opportunities exist to explore the potential of probiotics, prebiotics, and dietary interventions in modulating the gut microbiome to alleviate symptoms and slow disease progression in rheumatoid arthritis. By leveraging the latest research findings and technologies, healthcare providers can offer patients more personalized and effective treatment options that address the root causes of their condition, ultimately improving their quality of life.
To wrap up
With this in mind, understanding the connection between gut health and rheumatoid arthritis opens up promising avenues for further research and potential treatment options. By focusing on improving the balance of gut bacteria, reducing intestinal inflammation, and maintaining a healthy gut lining, individuals with rheumatoid arthritis may be able to alleviate symptoms and improve their quality of life.
It is crucial for healthcare providers and individuals living with rheumatoid arthritis to recognize the significance of gut health in managing this autoimmune condition. By taking proactive steps to support a healthy gut, such as adopting a balanced diet, managing stress, and incorporating probiotics, individuals may experience relief from inflammation and joint pain associated with rheumatoid arthritis. Overall, prioritizing gut health could be a game-changer in the treatment and management of this chronic condition.
FAQ
Q: What is the link between gut health and rheumatoid arthritis?
A: Research suggests that there is a strong connection between gut health and rheumatoid arthritis. The balance of bacteria in the gut, known as the gut microbiome, plays a crucial role in regulating the immune system. Disruptions in the gut microbiome can lead to inflammation, which is a key factor in the development and progression of rheumatoid arthritis.
Q: How does gut health influence rheumatoid arthritis?
A: The gut microbiome produces metabolites and other substances that can either promote or suppress inflammation in the body. Imbalances in the gut microbiome can lead to the production of pro-inflammatory compounds, which can exacerbate the symptoms of rheumatoid arthritis. Maintaining a healthy gut through a balanced diet, probiotics, and other lifestyle factors can help manage inflammation and improve symptoms of rheumatoid arthritis.
Q: What steps can be taken to improve gut health for individuals with rheumatoid arthritis?
A: To support gut health and potentially reduce inflammation associated with rheumatoid arthritis, individuals can consider incorporating probiotic-rich foods such as yogurt, kefir, and sauerkraut into their diets. Eating a diverse range of fruits, vegetables, whole grains, and lean proteins can also promote a healthy gut microbiome. Additionally, reducing stress, getting regular exercise, and staying hydrated can all contribute to overall gut health and potentially help manage symptoms of rheumatoid arthritis.