What Are The Key Differences Between Osteoarthritis And Rheumatoid Arthritis?
It’s crucial to understand the important differences between osteoarthritis (OA) and rheumatoid arthritis (RA) as they are both common types of arthritis but require different treatments. Osteoarthritis is the most common type of arthritis, affecting millions worldwide, while rheumatoid arthritis is an autoimmune disease that can cause severe joint damage and disability if not managed properly.
Key Takeaways:
- Osteoarthritis: It is a degenerative joint disease caused by wear and tear on joints over time.
- Rheumatoid Arthritis: It is an autoimmune disease where the body’s immune system attacks its own joints.
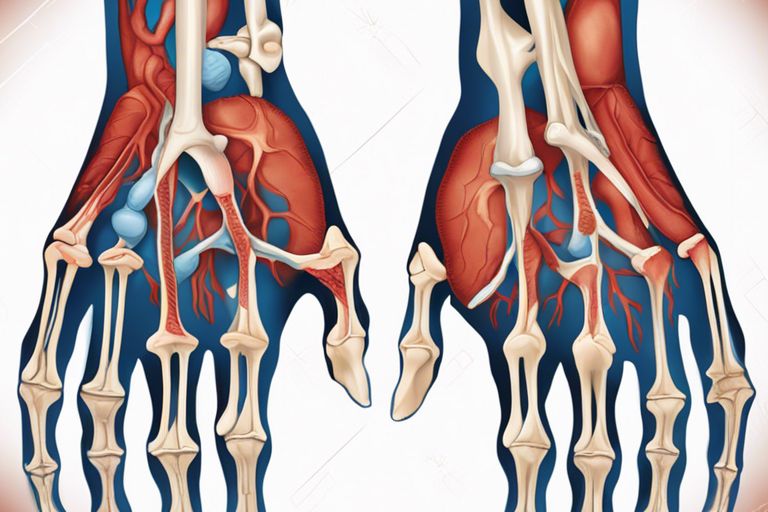
- Joint Involvement: Osteoarthritis typically affects weight-bearing joints, while rheumatoid arthritis commonly affects small joints in the hands and feet.
- Symptoms: Osteoarthritis symptoms usually include pain and stiffness in the affected joint, while rheumatoid arthritis symptoms may also include fatigue, fever, and weight loss.
- Treatment: Osteoarthritis is usually managed with pain relievers and lifestyle modifications, whereas rheumatoid arthritis requires disease-modifying antirheumatic drugs (DMARDs) and other medications to control inflammation.
- Onset: Osteoarthritis typically develops with age and is more common in older adults, while rheumatoid arthritis can develop at any age.
- Progression: Osteoarthritis progresses slowly over time, while rheumatoid arthritis can progress rapidly and cause joint deformities if left untreated.
Defining Osteoarthritis
Little is known about Osteoarthritis, commonly referred to as OA, a degenerative joint disease that affects millions of people worldwide. This chronic condition primarily targets the joints, causing pain, stiffness, and impaired mobility. Unlike Rheumatoid Arthritis (RA), which is an autoimmune disorder, OA is characterized by the breakdown of cartilage in the joints.
Pathophysiology of Osteoarthritis
To understand Osteoarthritis, we must probe into its pathophysiology. OA occurs when the protective cartilage that cushions the ends of bones wears down over time. As a result, the bones rub against each other, leading to pain, swelling, and reduced joint motion. This degenerative process can affect any joint in the body but commonly occurs in the knees, hips, hands, and spine.
Risk Factors and Demographics
An individual’s risk of developing OA is influenced by various factors such as age, obesity, joint injury, and genetics. Older adults are more susceptible to OA due to the natural wear and tear of joints over time. Additionally, excess body weight puts added stress on the joints, increasing the likelihood of cartilage damage. Joint injuries, especially those sustained during sports or accidents, can accelerate the onset of OA. Genetics also play a role, as certain inherited traits may predispose individuals to this condition. Assume that engaging in repetitive activities that strain the joints can exacerbate the risk of OA.
Any person, regardless of age, gender, or lifestyle, can develop Osteoarthritis. However, certain demographics, such as individuals over 50 years old, women, and athletes, are more prone to developing this degenerative joint disease. Assume that maintaining a healthy weight, staying physically active, and avoiding joint injuries can help reduce the risk of OA.
Common Symptoms of Osteoarthritis
One of the hallmark symptoms of Osteoarthritis is joint pain that worsens with activity and improves with rest. Stiffness in the affected joints, especially after periods of inactivity, is also a common complaint among individuals with OA. Swelling and a sensation of grating or grinding in the joint may accompany these symptoms.
This chronic condition can significantly impact a person’s quality of life, making daily activities challenging and painful. The progressive nature of OA can lead to joint deformities and permanent disability if left untreated. It is imperative to recognize these symptoms early on and seek medical evaluation to prevent further joint damage. Diagnosis and management of Osteoarthritis are crucial in mitigating its long-term effects on joint health.
Defining Rheumatoid Arthritis
Keep in mind that rheumatoid arthritis is a chronic inflammatory disorder that primarily affects the joints. Unlike osteoarthritis, which is a degenerative joint disease, rheumatoid arthritis is an autoimmune condition where the body’s immune system mistakenly attacks its own tissues, leading to inflammation, pain, and potential joint damage.
Pathophysiology of Rheumatoid Arthritis
For individuals with rheumatoid arthritis, the immune system targets the synovium, the membrane that lines the joints. This results in inflammation and thickening of the synovium, leading to joint pain, stiffness, and swelling. Over time, this persistent inflammation can cause cartilage and bone damage, ultimately affecting joint function and mobility.
Furthermore, in rheumatoid arthritis, the immune system can also attack other organs and tissues in the body, such as the heart, lungs, and eyes. This systemic inflammation can contribute to a range of complications beyond joint-related symptoms.
Genetic and Environmental Factors
Any discussion of rheumatoid arthritis must include the role of genetic and environmental factors in the development of the condition. It is believed that a combination of genetic predisposition and environmental triggers, such as infections or smoking, can lead to the onset of rheumatoid arthritis. Assume that certain genes, like HLA-DRB1, play a significant role in increasing susceptibility to the disease.
Rheumatoid arthritis can also be triggered by environmental factors like smoking, which is known to exacerbate the immune response and increase inflammation in the body. Additionally, exposure to certain infections or pollutants may contribute to the development of the condition. Assume that a combination of these factors can significantly increase the risk of developing rheumatoid arthritis.
Common Symptoms of Rheumatoid Arthritis
One of the hallmark symptoms of rheumatoid arthritis is joint pain and swelling, typically affecting multiple joints simultaneously. Patients may also experience morning stiffness that lasts for more than an hour, along with fatigue and general malaise. The inflammation associated with rheumatoid arthritis can lead to warmth and redness in the affected joints.
Arthritis in rheumatoid arthritis is often symmetrical, meaning that it affects the same joints on both sides of the body. In addition to joint symptoms, some individuals with rheumatoid arthritis may develop extra-articular manifestations, such as rheumatoid nodules or inflammation in other organs.
Diagnostic Criteria for Rheumatoid Arthritis
For a diagnosis of rheumatoid arthritis, healthcare providers typically follow the 2010 American College of Rheumatology/European League Against Rheumatism classification criteria. These criteria take into account joint involvement, serology, acute phase reactants, duration of symptoms, and the presence of autoantibodies like rheumatoid factor and anti-citrullinated protein antibodies (ACPAs).
A thorough clinical evaluation, including physical examination, imaging studies, and laboratory tests, is crucial for confirming a diagnosis of rheumatoid arthritis. Prompt diagnosis and initiation of appropriate treatment are crucial in managing the disease and preventing long-term joint damage and disability.
Comparing Onset and Progression
Not all types of arthritis are the same. Osteoarthritis and rheumatoid arthritis, despite both affecting the joints, have different onset patterns and progressions.
| Osteoarthritis | Rheumatoid Arthritis |
|
To start, osteoarthritis typically develops slowly over time. It is commonly seen in older individuals, with joint pain and stiffness worsening progressively. Symptoms may initially appear in one or several joints, such as the knees or hips, due to wear and tear on the cartilage. |
To start, rheumatoid arthritis can strike at any age, often between 30 and 60 years old. It tends to be more aggressive, with symptoms appearing suddenly and affecting multiple joints symmetrically. The inflammation is a hallmark of this autoimmune disease, leading to pain, swelling, and fatigue. |
Onset of Symptoms
For osteoarthritis, the onset of symptoms is usually linked to overuse of the joints or previous injuries. This degenerative type of arthritis manifests as stiffness and discomfort after activities, which gradually worsen with time. The pain in osteoarthritis is typically worse at the end of the day or after prolonged periods of rest.
For rheumatoid arthritis, the sudden onset of symptoms might include joint pain, swelling, and morning stiffness that lasts for more than an hour. Individuals may also experience fatigue, weight loss, and a general feeling of malaise. The systemic nature of this disease sets it apart from osteoarthritis in terms of the overall impact on the body.
Disease Progression and Joint Involvement
For osteoarthritis, progression is slow and typically involves the deterioration of the cartilage in the affected joints. As the condition advances, bone spurs may develop, leading to further pain and limitations in movement. While osteoarthritis primarily affects weight-bearing joints, such as knees, hips, and spine, it can also involve the fingers and thumbs.
For rheumatoid arthritis, the disease progression can be rapid and aggressive, impacting multiple joints simultaneously. The inflammation associated with rheumatoid arthritis not only damages the cartilage but can also affect surrounding tissues and organs. In severe cases, joint deformities may occur, limiting mobility and function.
Symptoms of rheumatoid arthritis can be debilitating, affecting the overall quality of life. Early diagnosis and treatment are crucial in managing the disease and preventing long-term joint damage. Regular monitoring by healthcare professionals and adherence to medication regimens can help individuals with rheumatoid arthritis lead active and fulfilling lives.
Differences in Joint Affected and Symptoms
Symmetry of Joint Involvement
Symptoms of joint involvement in osteoarthritis and rheumatoid arthritis can help differentiate between the two conditions. In osteoarthritis, the joint symptoms are often unilateral, affecting one side of the body. On the other hand, rheumatoid arthritis typically presents with bilateral joint involvement, affecting the same joints on both sides of the body.
Nature of Pain and Stiffness
The nature of pain and stiffness in osteoarthritis and rheumatoid arthritis can vary significantly. In osteoarthritis, the pain is usually localized to the affected joint and is often worse with activity. Stiffness tends to be more pronounced after periods of rest and improves with movement. In contrast, rheumatoid arthritis is characterized by symmetrical joint pain and stiffness, typically worse in the morning and improving throughout the day.
For instance, in rheumatoid arthritis, joint stiffness can last for an hour or more in the morning, a hallmark feature that distinguishes it from osteoarthritis.
Presence of Systemic Symptoms
Presence of systemic symptoms can also differentiate between osteoarthritis and rheumatoid arthritis. While osteoarthritis primarily affects the joints, rheumatoid arthritis is a systemic autoimmune disorder that can involve multiple organ systems in addition to the joints. Patients with rheumatoid arthritis may experience fatigue, fever, weight loss, and overall feelings of malaise.
Any presence of systemic symptoms should prompt further evaluation to rule out rheumatoid arthritis or other autoimmune conditions.

Imaging and Laboratory Findings
Despite both osteoarthritis (OA) and rheumatoid arthritis (RA) being chronic conditions that affect the joints, they have distinct differences in terms of imaging and laboratory findings that can aid in their diagnosis and management.
Radiographic Distinctions
To differentiate between OA and RA, physicians often rely on imaging studies such as X-rays. In OA, joint space narrowing, osteophyte formation, and subchondral sclerosis are typical findings. These changes are localized to the affected joint and tend to worsen over time as the condition progresses. In contrast, RA typically presents with symmetric joint involvement, periarticular osteopenia, and erosions at joint margins. These erosions are indicative of the inflammatory nature of RA, as opposed to the degenerative changes seen in OA.
It is important to note that while imaging findings can provide valuable information, they should always be interpreted in conjunction with clinical symptoms and other diagnostic tests to accurately diagnose and differentiate between OA and RA.
Blood Tests and Biomarkers
On the laboratory front, blood tests play a crucial role in distinguishing between OA and RA. In RA, elevated levels of rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies are commonly seen. These biomarkers are indicative of autoimmune activity and can help confirm the diagnosis of RA. On the other hand, these markers are typically negative in OA, as it is primarily a degenerative condition with no autoimmune component.
Imaging and laboratory findings are imperative tools in the diagnostic process of arthritis, providing valuable insights into the underlying pathophysiology of the condition and guiding the treatment approach. It is important for healthcare providers to thoroughly evaluate these findings in conjunction with clinical symptoms to ensure an accurate diagnosis and appropriate management plan for patients.
Treatment Options and Management
Your treatment options for osteoarthritis and rheumatoid arthritis can vary depending on the severity of your condition and other factors. It’s crucial to work closely with your healthcare provider to develop a comprehensive treatment plan that suits your specific needs.
Non-pharmacologic Therapies
Nonpharmacologic therapies play a fundamental role in managing arthritis symptoms. These may include physical therapy, occupational therapy, weight management, and hot or cold therapy. Physical therapy can help improve joint function and reduce pain, while occupational therapy focuses on making daily tasks easier to perform.
Regular exercise is also key in maintaining joint flexibility and strength. Low-impact activities like swimming, walking, or yoga can be particularly beneficial for individuals with arthritis, as they help improve mobility without putting excessive strain on the joints.
Pharmacologic Treatments
An effective pharmacologic treatment plan may include nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, disease-modifying antirheumatic drugs (DMARDs), and biologic response modifiers. NSAIDs can help reduce inflammation and pain, while DMARDs and biologics target the underlying causes of rheumatoid arthritis.
Any pharmacologic treatment should be carefully monitored by your healthcare provider to assess its efficacy and any potential side effects. It’s vital to communicate any concerns or changes in your symptoms to ensure the most appropriate medication regimen.
Surgical Interventions
Treatments for severe cases of arthritis may involve surgical interventions such as joint replacement or arthroscopy. Joint replacement surgery, including hip or knee replacement, can help restore function and reduce pain in damaged joints, improving overall quality of life for the patient.
Therapies such as arthroscopy may be recommended for diagnostic purposes or to address specific joint issues. These minimally invasive procedures can help healthcare providers visualize and treat joint problems with smaller incisions and faster recovery times.
Lifestyle and Home Remedies
On top of medical treatments, lifestyle changes and home remedies can complement your arthritis management plan. Maintaining a healthy weight, avoiding high-impact activities, and incorporating joint-friendly exercises into your routine can help reduce joint strain and improve your overall well-being.
Regular application of heat or cold packs to painful joints can provide temporary relief from discomfort and inflammation. Additionally, using assistive devices like braces or splints can support weakened joints and improve stability during daily activities.
The Role of Occupational and Physical Therapy
To enhance your treatment plan, occupational and physical therapy can play a crucial role in managing arthritis symptoms and improving joint function. Occupational therapists can help you adapt your home or work environment to reduce joint stress, while physical therapists can develop personalized exercise programs to enhance mobility and strength.
Interventions such as these can empower individuals with arthritis to take an active role in their treatment and self-care. By learning proper techniques for movement and joint protection, you can better manage your symptoms and maintain independence in daily activities.
Impact on Quality of Life and Prognosis
Many factors contribute to the impact of osteoarthritis and rheumatoid arthritis on an individual’s quality of life and prognosis. These factors go beyond physical symptoms and encompass emotional, social, employment, and long-term outcomes.
Emotional and Social Considerations
The emotional and social impact of osteoarthritis and rheumatoid arthritis can be significant, affecting relationships, mental well-being, and overall quality of life. Living with chronic pain, fatigue, and physical limitations can lead to feelings of isolation, anxiety, and depression. Additionally, the unpredictable nature of flare-ups and the need for assistance with daily tasks can strain relationships with family and friends.
Support from healthcare providers, counselors, support groups, and loved ones can play a crucial role in managing the emotional and social challenges of arthritis. Open communication, setting realistic expectations, and seeking professional help when needed are important steps in addressing these aspects of the condition.
Employment and Disability
Impact of arthritis on employment and disability can vary depending on the severity of the condition, physical demands of the job, and access to supportive measures. Individuals with severe arthritis may struggle to maintain full-time employment due to pain, fatigue, and physical limitations. In some cases, accommodations such as ergonomic workstations, flexible hours, or job modifications may be necessary to enable individuals to continue working.
Emotional and financial support is imperative for individuals navigating the challenges of balancing work and arthritis-related disability. Accessing disability benefits, vocational rehabilitation programs, and workplace accommodations can help individuals maintain their independence and financial stability while managing the impact of arthritis on their ability to work.
Long-term Outcomes
With proper management and treatment, individuals with osteoarthritis and rheumatoid arthritis can experience improved long-term outcomes and quality of life. Early diagnosis, tailored treatment plans, regular monitoring, and lifestyle modifications can help slow disease progression, reduce symptoms, and improve overall well-being over time.
Long-term outcomes may be influenced by factors such as disease activity, response to treatment, comorbidities, and adherence to self-care strategies. Regular follow-ups with healthcare providers, ongoing education about the condition, and an emphasis on holistic care can contribute to better long-term outcomes for individuals with arthritis.
Coping Strategies and Support Networks
Strategies for coping with arthritis include adopting a positive mindset, engaging in regular physical activity, maintaining a healthy diet, and seeking support from healthcare professionals, family, and friends. Building strong support networks, staying informed about treatment options, and developing effective coping strategies can empower individuals to better manage the challenges of living with arthritis.
Coping mechanisms such as mindfulness techniques, journaling, relaxation exercises, and participating in support groups can help individuals reduce stress, improve mood, and enhance their overall well-being. By proactively addressing the emotional, social, and physical aspects of arthritis, individuals can enhance their quality of life and prognosis in the long term.
Summing up
Drawing together the key differences between osteoarthritis and rheumatoid arthritis, it is evident that the two conditions have distinct characteristics that set them apart. Osteoarthritis is primarily a degenerative joint disease caused by wear and tear on the joints, while rheumatoid arthritis is an autoimmune disorder that causes inflammation and joint damage. The age of onset, risk factors, symptoms, and treatment approaches vary between the two conditions, making it crucial for healthcare professionals to accurately diagnose and differentiate between them.
Understanding the disparities between osteoarthritis and rheumatoid arthritis is vital for providing appropriate care and management strategies for individuals affected by these conditions. While both can result in joint pain and stiffness, the underlying causes and mechanisms of the diseases are fundamentally different. By recognizing the key differences, healthcare providers can develop tailored treatment plans that address the specific needs of patients living with osteoarthritis or rheumatoid arthritis, ultimately improving their quality of life and overall well-being.
FAQ
Q: What Are the Key Differences Between Osteoarthritis and Rheumatoid Arthritis?
A: Osteoarthritis is a degenerative joint disease that primarily affects the cartilage in the joints, while rheumatoid arthritis is an autoimmune disease that causes inflammation in the lining of the joints.
Q: How do the Symptoms of Osteoarthritis Differ from Rheumatoid Arthritis?
A: Symptoms of osteoarthritis include joint pain, stiffness, and limited range of motion, usually worsening with activity. Rheumatoid arthritis symptoms include joint pain, swelling, warmth, and morning stiffness that can last for hours.
Q: Are there Differences in Treatment Approaches for Osteoarthritis and Rheumatoid Arthritis?
A: Yes, treatment for osteoarthritis focuses on pain management, improving joint function, and possibly surgery in severe cases. Rheumatoid arthritis treatment aims to reduce inflammation, slow the progression of the disease, and preserve joint function through medications, physical therapy, and sometimes surgery.

0 comments