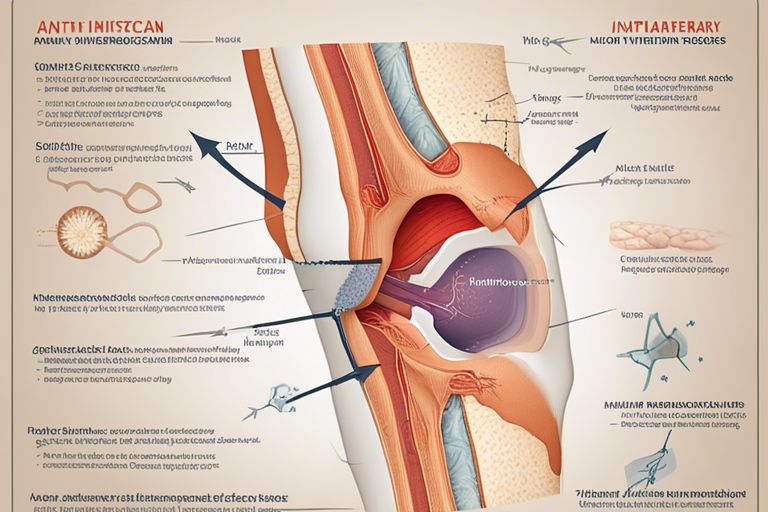
Rheumatoid arthritis is a chronic autoimmune condition that causes inflammation, pain, and swelling in the joints. During flare-ups, individuals experience intensified symptoms, making it crucial to find effective ways to manage the condition. While traditional medications can be highly beneficial, exploring alternative remedies can offer additional support in managing rheumatoid arthritis flare-ups.
Key Takeaways:
- Diet plays a crucial role: Eating anti-inflammatory foods like fish, nuts, fruits, and vegetables can help reduce inflammation and manage rheumatoid arthritis flare-ups.
- Supplements can be beneficial: Omega-3 fatty acids, turmeric, and ginger supplements have shown anti-inflammatory properties that can aid in managing symptoms of rheumatoid arthritis.
- Acupuncture and acupressure: These alternative therapies can help reduce pain and improve mobility in rheumatoid arthritis patients during flare-ups.
- Physical therapy exercises: Regular low-impact exercises prescribed by a physical therapist can help strengthen muscles, improve flexibility, and reduce pain associated with rheumatoid arthritis flare-ups.
- Mind-body practices: Techniques like yoga, meditation, and deep breathing exercises can help manage stress, improve mental well-being, and potentially reduce the frequency or severity of flare-ups.
- Heat and cold therapy: Applying heat or cold packs to affected joints can help reduce inflammation, numb pain, and improve mobility during rheumatoid arthritis flare-ups.
- Consult with healthcare providers: It’s important to discuss any alternative remedies with your healthcare team to ensure they complement your current treatment plan and do not interfere with medications prescribed for managing rheumatoid arthritis.
Understanding Rheumatoid Arthritis Flare-ups
Now, when it comes to managing rheumatoid arthritis flare-ups, understanding the triggers and symptoms is crucial. Flare-ups are episodes of increased disease activity, leading to heightened inflammation and pain in the joints. Recognizing the factors that can trigger these flare-ups is vital in mitigating their impact on daily life.
Triggers and Symptoms
To effectively manage rheumatoid arthritis flare-ups, it’s important to identify potential triggers that can exacerbate the condition. Common triggers include stress, poor sleep, infections, changes in weather, and certain foods. The symptoms of a flare-up can vary from person to person but often include increased joint pain, swelling, stiffness, fatigue, and difficulty with daily activities.
Understanding the triggers and symptoms of rheumatoid arthritis flare-ups can help individuals take proactive measures to prevent and manage these episodes. By learning to recognize the early signs of a flare-up, such as increased joint pain and fatigue, individuals can adjust their treatment plan accordingly and seek medical assistance if needed. It is vital to work closely with healthcare providers to develop a comprehensive management strategy tailored to each individual’s needs.
Conventional Treatments for Rheumatoid Arthritis
There’s a range of conventional treatments available for managing rheumatoid arthritis, each aimed at reducing inflammation, alleviating pain, and slowing down the progression of the disease. These treatments are typically prescribed by healthcare providers and may include medication options, physical therapy, and lifestyle modifications.
Medication Options
Treatments for rheumatoid arthritis often begin with medications like non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and disease-modifying antirheumatic drugs (DMARDs) such as methotrexate. These medications help to reduce inflammation, relieve pain, and prevent joint damage. In more severe cases, biologic response modifiers, which target specific parts of the immune system responsible for inflammation, may be prescribed.
Physical Therapy and Exercise
Conventional treatments for rheumatoid arthritis may also include physical therapy and exercise regimens. Physical therapy can help improve joint function, flexibility, and strength, while exercise can help maintain overall health and prevent muscle atrophy. Regular physical activity has been shown to reduce joint pain and stiffness in individuals with rheumatoid arthritis.
For instance, low-impact exercises such as swimming, biking, and yoga can be particularly beneficial for individuals with rheumatoid arthritis. These activities can help improve cardiovascular health, increase joint range of motion, and promote muscle strength without putting excessive stress on the joints.

Nutritional Strategies in Managing Flare-ups
After experiencing a rheumatoid arthritis flare-up, incorporating specific nutritional strategies can play a crucial role in managing symptoms and promoting overall well-being. A balanced diet rich in anti-inflammatory foods and targeted dietary supplements can help reduce inflammation, alleviate pain, and support joint health.
Anti-inflammatory Foods
To combat inflammation and potentially ease rheumatoid arthritis symptoms during a flare-up, focusing on incorporating anti-inflammatory foods into your diet is important. Foods such as fatty fish (salmon, mackerel, sardines), turmeric, ginger, green leafy vegetables, nuts, and seeds are known for their anti-inflammatory properties. These foods contain important nutrients and compounds that can help reduce inflammation in the body and provide relief from joint pain.
Additionally, incorporating fruits like berries, cherries, and oranges can also contribute to lowering inflammation levels. These fruits are rich in antioxidants, which help combat oxidative stress and inflammation in the body. By including a variety of anti-inflammatory foods in your diet, you can support your body’s natural ability to manage rheumatoid arthritis flare-ups.
Dietary Supplements
One way to enhance your nutritional intake and support your body during rheumatoid arthritis flare-ups is through the use of dietary supplements. Supplements such as omega-3 fatty acids, turmeric extract, ginger extract, and vitamin D have been studied for their anti-inflammatory and pain-relieving properties. These supplements can help reduce inflammation, alleviate joint pain, and improve overall joint function.
This targeted approach to dietary supplementation allows for a more concentrated intake of key nutrients that support joint health and reduce inflammation. However, it is important to consult with a healthcare provider before starting any new supplements, as they can interact with medications or have contraindications for certain health conditions. Supplements should complement a balanced diet and not replace it entirely.
Mind-Body Techniques
Many individuals living with rheumatoid arthritis find relief through mind-body techniques that focus on promoting relaxation and well-being. These methods can help in managing flare-ups and reducing the overall impact of the disease on daily life.
Stress Reduction Methods
Reduction of stress is crucial for individuals with rheumatoid arthritis, as stress can exacerbate symptoms and trigger flare-ups. Techniques such as deep breathing exercises, progressive muscle relaxation, and biofeedback can help in lowering stress levels and promoting a sense of calm.
Engaging in activities such as yoga, tai chi, or qigong can also be beneficial as they combine physical movement with mindfulness, promoting relaxation and reducing stress on both the body and mind.
The Role of Mindfulness and Meditation
For individuals with rheumatoid arthritis, incorporating mindfulness and meditation into their daily routine can have a profound impact on managing the disease. Mindfulness practices encourage staying present in the moment, reducing anxiety about the future and negative emotions surrounding the condition.
MindBody techniques like guided imagery and body scanning can help individuals connect with their bodies, identify areas of tension, and release stress and discomfort. By cultivating a state of mindfulness, individuals can better cope with the challenges of rheumatoid arthritis flare-ups and improve their overall quality of life.
Herbal Remedies for Rheumatoid Arthritis
Efficacy of Herbal Supplements
Keep in mind that the efficacy of herbal supplements in managing rheumatoid arthritis flare-ups can vary from individual to individual. Some people report positive outcomes with the use of certain herbs like turmeric, ginger, and Boswellia serrata. These herbs are believed to have anti-inflammatory properties that may help reduce joint pain and swelling associated with rheumatoid arthritis.
However, it is imperative to note that scientific research on the effectiveness of herbal remedies for rheumatoid arthritis is limited. While some studies suggest potential benefits, more research is needed to confirm their efficacy and determine the appropriate dosage for optimal results.
Potential Risks and Interactions
An important consideration when using herbal remedies for rheumatoid arthritis is the potential risks and interactions they may have. Some herbs, such as St. John’s Wort and garlic, can interact with certain medications commonly prescribed for rheumatoid arthritis, potentially reducing their effectiveness or causing adverse reactions.
Rheumatoid arthritis patients should always consult with their healthcare provider before incorporating herbal supplements into their treatment regimen. It is crucial to discuss any existing medications and health conditions to ensure safe and effective use of herbal remedies.
Physical Modalities and Complementary Therapies
All individuals living with rheumatoid arthritis know the challenges that come with managing flare-ups. In addition to conventional treatments, exploring alternative remedies such as physical modalities and complementary therapies can offer relief and improve overall well-being.
Acupuncture and Acupressure
Therapies such as acupuncture and acupressure have gained popularity for their potential in alleviating RA symptoms. Acupuncture involves the insertion of thin needles into specific points on the body to help restore balance in the flow of energy, while acupressure applies pressure to these same points. Research suggests that these techniques may help reduce pain, inflammation, and improve joint mobility in individuals with RA.
Therapies like acupuncture and acupressure are considered safe when performed by trained practitioners. However, it is necessary to consult with a healthcare provider before trying these modalities to ensure they complement your current treatment plan and do not interfere with any medications.
Massage and Chiropractic Care
An array of individuals with rheumatoid arthritis find relief through massage and chiropractic care. Massage therapy involves manipulating soft tissues to reduce muscle tension, improve circulation, and promote relaxation. Chiropractic care focuses on spinal adjustments to enhance joint function and reduce pain. Both modalities can contribute to managing RA symptoms and enhancing overall quality of life.
An important consideration when incorporating massage and chiropractic care into your RA management plan is to ensure that the therapists are experienced in working with individuals with arthritis. Communicate openly about your condition and any specific areas of concern to tailor the treatments to your needs and avoid any potential complications.
Heat and Cold Applications
Modalities such as heat and cold therapy can be valuable tools in managing RA flare-ups. The application of heat, through techniques like warm baths, heating pads, or warm compresses, can help relax muscles, reduce joint stiffness, and alleviate pain. Conversely, cold therapy, using ice packs or cold compresses, can help alleviate inflammation and swelling in affected joints.
Any temperature therapy should be used cautiously, as excessive heat or cold exposure can potentially worsen symptoms or cause tissue damage. It is recommended to consult with a healthcare provider to determine the most suitable approach and duration for applying heat and cold therapies based on individual needs and preferences.
Living with Rheumatoid Arthritis
Despite the challenges of managing rheumatoid arthritis, individuals can find ways to improve their quality of life and reduce the impact of flare-ups. Lifestyle modifications, patient support, and education play critical roles in helping individuals navigate their daily lives with this chronic condition.
Lifestyle Modifications
One of the key aspects of managing rheumatoid arthritis is making lifestyle modifications to accommodate the symptoms and limitations of the disease. This can include implementing an exercise routine tailored to improve joint flexibility and strength, as well as adopting a balanced diet to maintain a healthy weight and reduce inflammation. Additionally, stress management techniques such as meditation or yoga can help alleviate the mental and emotional toll of living with a chronic illness.
Patient Support and Education
Modifications in lifestyle are crucial, but so is having a strong support system and access to relevant patient support and education. Joining support groups or online communities can provide individuals with rheumatoid arthritis a sense of belonging and understanding, while also offering valuable tips and insights from others sharing similar experiences. Moreover, staying informed about the latest treatment options and self-care strategies through educational resources can empower patients to take an active role in managing their condition.
Rheumatoid arthritis can be a challenging condition to live with, but with the right patient support and education, individuals can gain a better understanding of their disease and learn how to effectively manage their symptoms. Empowering patients with knowledge and a strong support network can ultimately lead to improved quality of life and better outcomes in the long run.
Conclusion
So, it is evident that there are various alternative remedies available for managing rheumatoid arthritis flare-ups. From incorporating anti-inflammatory foods in your diet to trying out acupuncture or yoga, there are plenty of options to explore. It is vital to remember that what works for one individual may not work for another, so it may require some trial and error to find the most effective remedy for you.
By being open to alternative remedies and working closely with your healthcare provider, you can develop a personalized approach to managing rheumatoid arthritis flare-ups that best suits your needs. Remember to prioritize self-care, listen to your body, and continue to explore different options to find what works best for you in managing your symptoms.
FAQ
Q: What are alternative remedies for managing rheumatoid arthritis flare-ups?
A: When dealing with rheumatoid arthritis flare-ups, there are several alternative remedies that can help manage symptoms. These include acupuncture, massage therapy, herbal supplements, and mind-body techniques such as yoga and meditation. It is important to consult with a healthcare provider before trying any alternative remedies to ensure they are safe and appropriate for your specific condition.
Q: Can diet and nutrition help with rheumatoid arthritis flare-ups?
A: Yes, diet and nutrition can play a role in managing rheumatoid arthritis flare-ups. Some foods, such as fatty fish, nuts, fruits, and vegetables, have anti-inflammatory properties that may help reduce inflammation and pain. Avoiding processed foods, sugars, and saturated fats is also important, as these can exacerbate inflammation. Consulting with a registered dietitian can help develop a nutrition plan tailored to your individual needs.
Q: Are there natural supplements that can help with rheumatoid arthritis flare-ups?
A: Some natural supplements have been found to have anti-inflammatory properties that may help manage rheumatoid arthritis flare-ups. These include turmeric, ginger, omega-3 fatty acids, and Boswellia. However, it is crucial to speak with a healthcare provider before taking any supplements, as they can interact with medications or exacerbate certain health conditions. Integrating supplements into your treatment plan should be done under medical supervision.